Microbicide effectivness derives from complex, multivariate interactions between properties of both the active ingredient and the delivery vehicle. There is a need within microbicide development to understand the collective effects this set of critical microbicide properties have upon in vivo effectiveness.
We have initiated use of deterministic biophysical methodology -- theoretical and experimental -- to track semen-borne HIV virions as they migrate from semen to mucosal surfaces and then into the underlying epithelium.
Theoretical Modeling
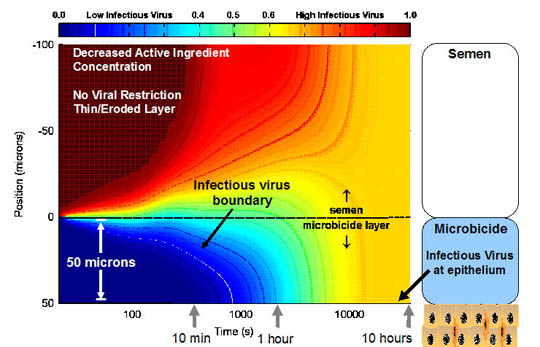
We have created a mathematical predictive model for the time and space dependence (time since ejaculation, distance from mucosal surface) of concentrations of virions and of anti-viral molecules, and the extent to which the virions are disabled before migrating to the mucosal surface. Inputs to the model will include data on: viral load in semen; initial concentration, mechanism and potency of the anti-viral molecules in the mucosal coating layer; and mobilities of HIV and the anti-HIV molecules in that layer and in semen.
Schematic of the mathematical model
This model adds to the understanding of the transport and neutralization processes that occur when semen-borne HIV contacts a microbicide mucosal coating layer, and how these processes are affected by the properties of both the microbicide and the biological environment. Outputs will enable inter-microbicide comparisions and lead to individual microbicide optimization.
Effective Microbicide: All infectious virus neutralized in semen
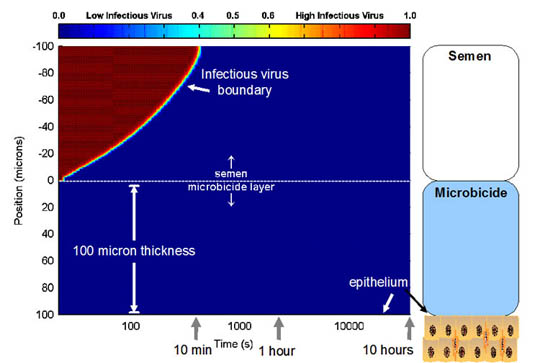
Active Ingredient Distribution: Release of anti-HIV agent into semen

Ineffective Microbicide : Infectious virus reaches epithelium in 20 minutes
In Vitro Experimental Model of HIV Transport
We developed a bioassay that simulates the in vivo configuration of semen and a microbicide formulation over vaginal epithelium. The assay measures the kinetics of viral transport across the gel layer, infectivity of virus that passes through it, and release of active ingredients from the layer.

A transwell chamber allows semen-borne HIV to migrate through a gel layer to a substrate material (e.g. porous membranes or tissue explants). The design of the chamber allows for sampling of each material to measure the concentrations of total HIV and active ingredient, and to remove fluid or tissue below the gel for use in assays to quantify infection.
